I am currently practicing in the state of Arizona as a licensed mental health therapist (i.e., LMHC), working within a behavioral health and integrated care setting. My scope of practice and billing ability are determined by my level of licensure and payor rules that are set by AHCCCS (Arizona Medicaid) and contracted managed care organizations. In Arizona, mental health therapists may bill under CPT, HCPCS and “H-codes,” depending on credentials. A person’s credentials directly affect reimbursement rates and provider service eligibility.
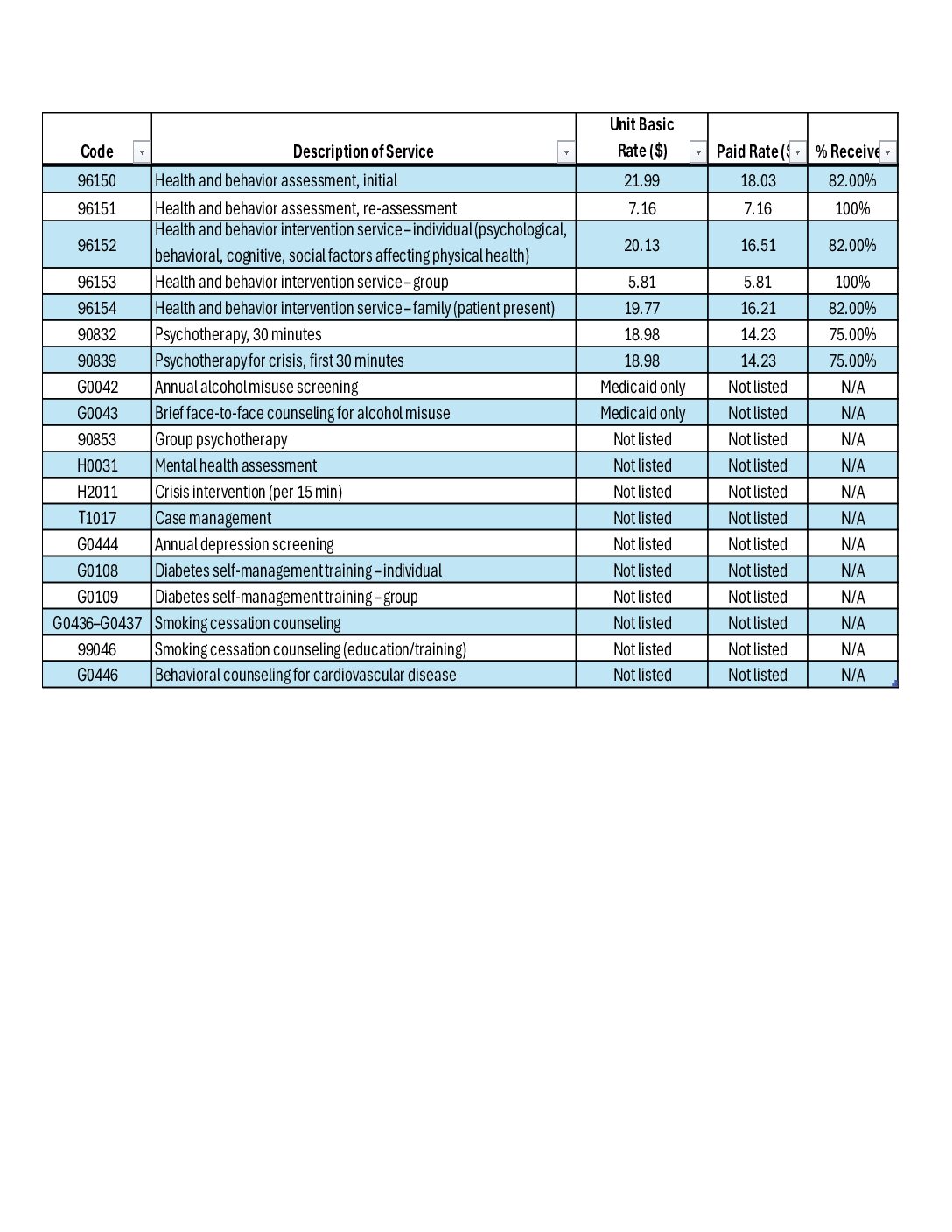
The chart referenced in this post (attached at the end of this discussion) outlines behavioral health, health and behavior assessment, and integrated care billing codes relevant to Arizona mental health therapists. It includes the code number, description of service, basic unit rate, paid rate, and percentage received where available. By reviewing this chart, the reader can clearly see which services are reimbursed at higher or lower percentages, which codes are fully reimbursed, and which services are either Medicaid-only or lack standardized public rates. This transparency highlights how reimbursement is not solely tied to clinical effort, but to payor policy, provider type, and service provided.
Analyzing the chart information provides several benefits. First, it allows both clinicians and organizations to make decisions about service delivery. Understanding which codes reimburse at 100% versus 75–82% helps prioritize sustainable services without compromising care quality. Second, it supports strategic planning for integrated care by identifying underutilized but billable services, such as health and behavior interventions, screenings, and group care. For my organization, this information can be used to optimize scheduling, improve documentation practices, and advocate for credentialing pathways that expand billing privileges.
Looking at the data incentives, add-on services include expanding group therapy offerings, integrating brief behavioral health screenings (depression, alcohol misuse, smoking cessation), and developing family-based or crisis-focused interventions. These services not only align with whole-person care models but also enhance patient outcomes, engagement, and retention, which can improve care while generating revenue.
A DBH-trained professional brings the value to bridge clinical care, billing literacy, integrated care models, and organizational strategy. This combination is essential for creating financially sustainable systems that improve access, quality, and outcomes.